Written by: Dr.
E. Fuller Torrey (Note: schizophrenia.com has
added the photos and some of the more recent medical research references
in this article)
History of the Scientific View on Schizophrenia
as a Brain Disorder: It has been suspected for over a century that schizophrenia
and manic-depressive disorder (bipolar disorder) are disorders of the brain.
In 1837, Dr. W.A.F. Browne, the best-known English psychiatrist of his
generation, wrote:
"Insanity, then, is inordinate or irregular, or impaired action
of the mind, of the instincts, sentiments, intellectual, or perceptive
powers, depending upon and produced by an organic change in the brain."
In that same year, Dr. Amariah Brigham, one of the founders of American
psychiatry, also wrote that insanity "is now considered a physical
disorder, a disease of the brain."
It would be 150 years, however, before these statements could be proven.
Since the early 1980s, with the availability of brain imaging techniques
and other developments in neuroscience, the evidence has become overwhelming
that schizophrenia and manic-depressive disorder are disorders of the
brain.
Additional research done during the past decade has revealed that schizophrenia is caused by a combination of genetic or biological predisposition as well as other factors such as prepregnancy factors, pregnancy stress, other prenatal factors, social stress, family stress or environmental stressors during a person's life. Research has now shown that children's and teen's brains are very sensitive to stress (up to 5 to 10 times more sensitive than adult brains) and can be damaged by frequent or ongoing stress.
To learn more about the causes of schizophrenia, and how to prevent it - read these two documents: Causes of Schizophrenia, Prevention of Schizophrenia.
A brief summary of some of the evidence that proves this point follows.
Significant Loss of Brain Gray Matter:
Individuals with schizophrenia, including those who have never been
treated, have a reduced volume of gray matter in the brain, especially
in the temporal and frontal lobes. Recently neuroscientists have detected
gray matter loss of up to 25% (in some areas). The damage started in
the parietal, or outer, regions of the brain but spread to the rest
of the brain over a five year period. Patients with the worst brain
tissue loss also had the worst symptoms, which included hallucinations,
delusions, bizarre and psychotic thoughts, hearing voices, and depression.
Please note that while there is significant loss of brain gray matter,
this is not a reason to lose all hope. In recent (September, 2004) group
of presentations and discussion we had with Dr. Daniel Weinberger and
other leading National Institute of Mental Health (NIMH) schizophrenia
researchers, we learned that there are reasons to believe that this
gray matter loss may be reversable. Moreover, the NIMH is currently
researching a drug that seems to have potential for reversing the cognitive
decline that is caused by schizophrenia, and there are many drug companies
also now researching in this area. It is anticipated that we will see
some significant announcements related to these develpments in the next
few years.
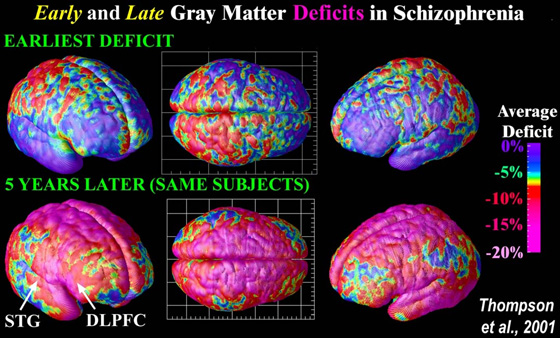
To see more images of brains that are suffering from schizophrenia, go to: Schizophrenia Brain Images. The Image Source is: Laboratory
of Neuro Imaging, UCLA, Derived
from high-resolution magnetic resonance images (MRI scans), the above
images were created after repeatedly scanning 12 schizophrenia subjects
over five years, and comparing them with matched 12 healthy controls,
scanned at the same ages and intervals. Severe loss of gray matter
is indicated by red and pink colors, while stable regions are in blue.
STG denotes the superior temporal gyrus, and DLPFC denotes the dorsolateral
prefrontal cortex. Note: This study was of Childhood onset schizophrenia
which occurs in 1 of every 40,000 people and is frequently a significantly
more aggressive form of schizophrenia (than later onset schizophrenia
which afflicts approximately 1 of every 100 people).
A Sample of Recent Relevant Research:
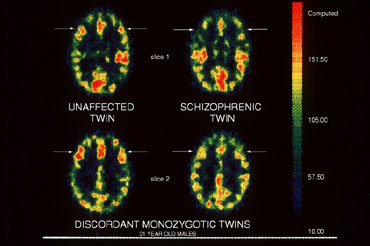
Enlaged Ventricles in the Brain:
Individuals with schizophrenia, including those who have never been
treated, typically have enlarged ventricles in the brain, as demonstrated
in over 100 studies to date.
above: MRI imaging showing differences in brain ventricle
size in twins - one schizophrenic, one not. (image courtesy NIH - Dr.
Daniel Weinberger, Clinical Brain Disorders Branch)
A Sample of Recent Relevant Research:
- Ventricular
enlargement in schizophrenia related to volume reduction of the thalamus,
striatum, and superior temporal cortex, Am J Psychiatry.
2004 Jan;161(1):154-6.
- Association
between minor physical anomalies and lateral ventricular enlargement
in childhood and adolescent onset schizophrenia,
Acta Psychiatr Scand. 2003 Aug;108(2):147-51
- Progressive
structural brain abnormalities and their relationship to clinical
outcome: a longitudinal magnetic resonance imaging study early in
schizophrenia.
Arch Gen Psychiatry. 2003 Jun;60(6):585-94.
- Cerebral
ventricular enlargement as a generalized feature of schizophrenia:
a distribution analysis on 502 subjects.,
Schizophr Res. 2000 Jul 7;44(1):25-34.
- Van Horn JD, McManus IC.
Ventricular enlargement in schizophrenia. A meta-analysis of studies
of the ventricle:brain ratio (VBR). British Journal of Psychiatry
160:687–697, 1992.
- Soares JC, Mann JJ. The
anatomy of mood disorders: review of structural neuroimaging studies.
Biological Psychiatry 41:86–106, 1997.
- Elkis H, Friedman L, Wise
A, et al. Meta-analyses of studies of ventricular enlargement and
cortical sulcal prominence in mood disorders. Comparisons with controls
or patients with schizophrenia. Archives of General Psychiatry 52:735–746,
1995.
Enlarged Amygdala: Individuals
with manic-depressive disorder have an enlarged amygdala and increased
numbers of white matter hyperintensities.
- Strakowski SM, DelBello MP, Sax KW, et al. Brain
magnetic resonance imaging of structural abnormalities in bipolar
disorder. Archives of General Psychiatry 56:254–260, 1999.
- Dupont RM, Jernigan TL, Heindel W, et al. Magnetic
resonance imaging and mood disorders: localization of white matter
and other subcortical abnormalities. Archives of General Psychiatry
52:747–755, 1995.
- Videbech P. MRI findings in patients with affective
disorder: a meta-analysis. Acta Psychiatrica Scandinavica 96:157–168,
1997.
Neurological Abnormalities: Individuals
with schizophrenia and manic-depressive disorder, including those who
have never been treated, have more neurological abnormalities, as shown
in over 25 studies.
Impaired Cognitive Function:
Individuals with schizophrenia and manic-depressive disorder, including
those who have never been treated, have more neuropsychological abnormalities
that impair their cognitive function, including such things as information
processing and verbal memory.
A Sample of Recent Relevant Research:
- Neuropsychological
deficits in children associated with increased familial risk for
schizophrenia, : Schizophr Res. 2004 Apr
1;67(2-3):123-30.
- Long-term
memory deficits in schizophrenia: primary or secondary dysfunction?
Neuropsychology. 2003 Oct;17(4):539-47.
- Convergence
of biological and psychological perspectives on cognitive coordination
in schizophrenia, Behav Brain Sci. 2003
Feb;26(1):65-82; discussion 82-137.
- A
prospective study of childhood neurocognitive functioning in schizophrenic
patients and their siblings, Am J Psychiatry.
2003 Nov;160(11):2060-2.
- Goldberg TE, Gold JM. Neurocognitive functioning
in patients with schizophrenia: an overview. In: Psychopharmacology:
The Fourth Generation of Progress, Bloom FE and Kupfer DJ (eds).
New York: Raven Press, 1995, pp. 1245–1257.
- Hoff AL, Shukla S, Aronson T, et al. Failure to
differentiate bipolar disorder from schizophrenia on measures of
neuropsychological function. Schizophrenia Research 3:253–260,
1990.
- Morice R. Cognitive inflexibility and pre-frontal
dysfunction in schizophrenia and mania. British Journal of Psychiatry
157:50–54, 1990.
Decreased Prefrontal Brain Function:
Individuals with schizophrenia, including those who have never been
treated, show decreased function of the prefrontal area, an area of
the brain that we use for planning and thinking about ourselves.
above: PET imaging showing areas of
brain activity in twins - one schizophrenic, one not. (image courtesy
Dr. Karen Berman, Clinical Brain Disorders Branch, NIMH, NIH)
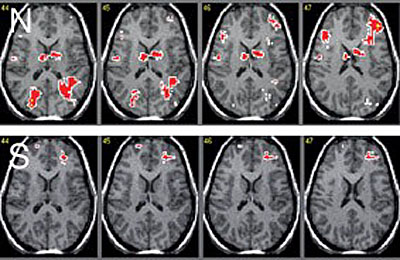
Above: Decreased brain activity
in schizophrenia subjects (S) compared to normal controls(N) in an
fMRI study examining executive functioning. Image courtesy of Prof.
Philip Ward, NISAD Cognitive Neuroscience Research Panel.
Impaired Awareness of Ilness: Approximately
50 percent of individuals with schizophrenia and manic-depressive disorder,
including those who have never been treated, have impaired awareness
of their own illness. This has been shown in at least 50 different studies.
Such individuals do not realize that they are sick, and they will, therefore,
usually not accept treatment voluntarily. Studies suggest that this
impaired awareness is probably related to the decreased function of
the prefrontal area of the brain.
These individuals are thus similar to some patients who have had a
stroke and, because of brain damage, are unaware of their disability
and deny it. The lack of awareness of illness in individuals with schizophrenia
and manic-depressive disorder is the most common reason that they do
not take their medication. [as can be seen in the research below, the
part of the brain that is resonsible for self-analysis seems to be one
of the areas most damaged by schizophrenia; the brain that is damaged,
cannot frequently recognize that it is damaged]. This is a problem is
because increasingly schizophrenia research is suggesting that the sooner
a person with this brain disease is treated, the better the outcome
for the person. Delays for treatment result in much worse outcome (see
recent research below).
A Sample of Recent Relevant Research:
Additional Information on the Disease Process of Schizophrenia:
|
|



